Breastfeeding is a skill that mothers or breastfeeding parents and babies have to learn. Read about feeding cues, how to attach the baby onto the breast, and comfortable positions to explore.
Starting to breastfeed
When you first start breastfeeding, you and your baby may take a while to pick up this new skill (NHS Start for Life, no date a). Your midwife should help in the early days. Anyone supporting with breastfeeding should ask permission if they think touching the mother or breastfeeding parent’s body will help with feeding (NICE, 2021).
Patience and experimenting will help you learn to recognise your baby’s feeding cues and find a position that is comfortable and works for you both.
If you need support with any aspect of breastfeeding, call our infant feeding support line on 0300 330 0700 to talk to a Breastfeeding Counsellor or go to one of our local groups. If you have met a BFC during one of our Antenatal Courses then they will have also given you details of the support they offer.
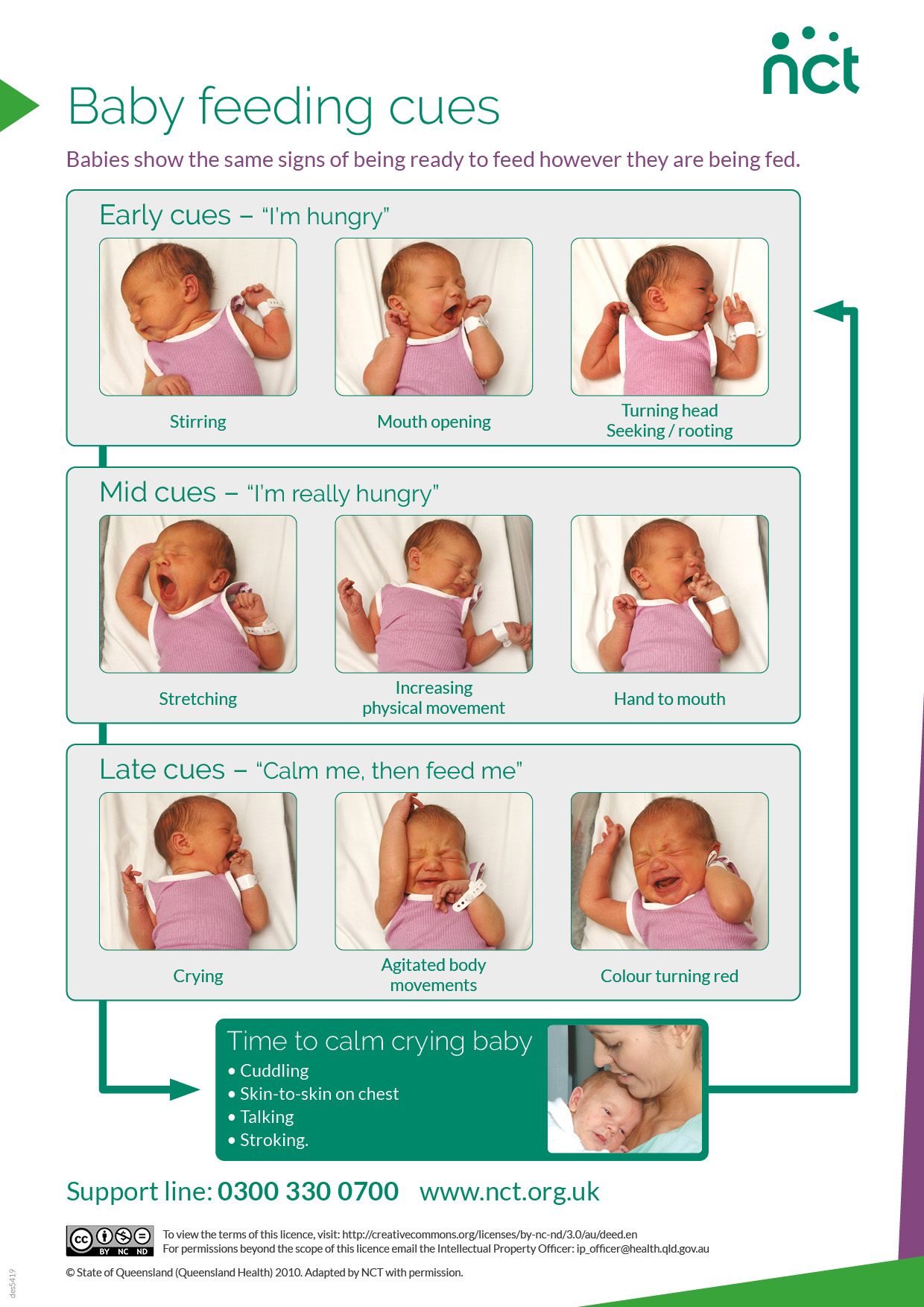
Feeding cues
Babies signal when they want a feed with cues. If you learn how to spot these early cues, your baby is more likely to attach and feed. If cues are missed, crying is the baby’s last attempt to signal wanting to feed.
If the baby is crying or upset, they need to be calmed before they are ready to feed.
Preparing to feed
- Most babies like to have their hands free to touch and stroke the breast. This helps reassure them that they are in the right place.
- Get comfortable before starting. If possible, have a drink or snack handy before sitting down.
- To start with, it’s best to get the baby attached to the breast first, and only add the support of a pillow if it’s needed. Otherwise, a pillow or support can prevent the baby’s body getting into the right position.
Attachment
Latching is how the baby attaches to the breast. When attachment is effective, the feed will be comfortable for the mother or breastfeeding parent and baby. Effective attachment prevents sore and cracked nipples and makes it easier for the baby to get milk (NHS Start for Life, no date a).
Getting the baby to latch on (NHS, 2022 a)

Make sure the baby is held close, with their head and body in a straight line, because it’s hard to swallow with a twisted neck.
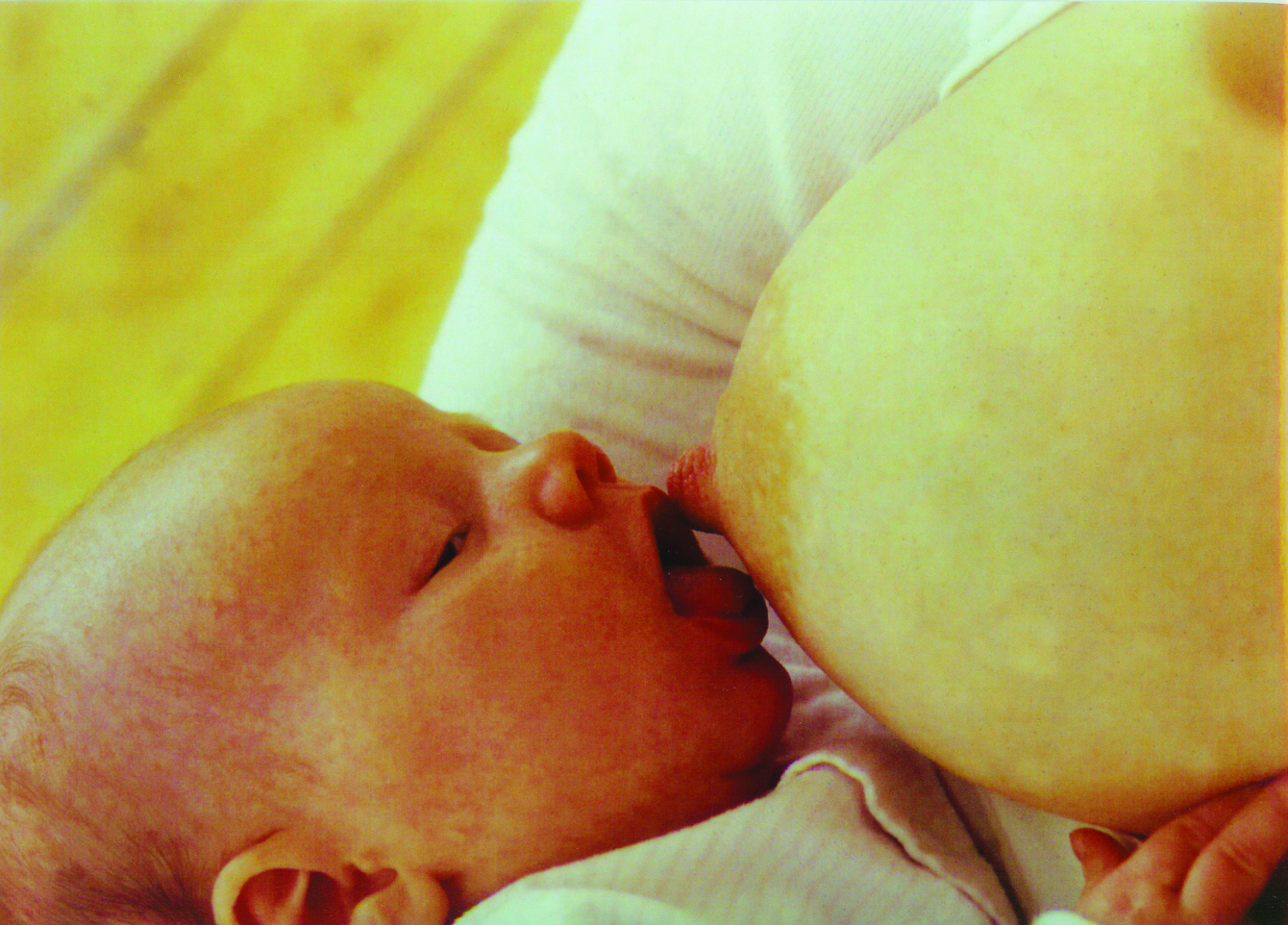
Bring the baby close to the breast. Avoid leaning the breast into the baby. Support the baby’s neck, shoulders and back. Do not hold the back of the head.

The baby’s nose should be level with the nipple, so that they need to tip their head back for the top lip to brush against the nipple. This will encourage them to open their mouth wide.

With the chin on the breast and mouth wide open, the baby should get a big mouthful of breast. This means the nipple goes right to the back of their mouth.
Signs that a baby is attached well could be (Breastfeeding Network, no date; NHS, 2022 a):
- More of the darker nipple skin visible above the baby’s top lip than below their bottom lip
- The baby’s cheeks are full and rounded
- It feels comfortable, although the first sucks and the let-down reflex might feel strong
- Swallowing can be seen and heard (although there will be pauses in swallowing).
- The baby comes off the breast on their own
- They produce plenty of wet and dirty nappies
The baby is not attached well if (Breastfeeding Network, no date; NHS, 2022 a):
- The initial discomfort of latching on doesn’t go away and continues through the feed
- Swallowing from the baby isn’t heard often, or at all
- The nipples look pinched or squashed after a feed
- The nipples become cracked or sore
- The baby starts to feed then pulls away or seems unsettled
Read our article ‘Is my baby feeding well?’ for more ways to tell if your baby is getting enough milk and feeding effectively. You can also call our Breastfeeding Counsellors on 0300 330 0700, every day of the year from 8am to midnight.
Breastfeeding positions
The way you hold your baby will affect how easy it is for them to breastfeed effectively. It’s good to try different positions to find what’s most comfortable and effective for you both. Here we share some common positions for getting started with breastfeeding.
Laid-back position
Research shows that the mother or breastfeeding person’s posture can either encourage or get in the way of the baby’s instinctive feeding behaviours (Coulson, 2012).
Usually, baby reflexes at the start of a feed help them find the breast, latch on and feed. These include moving their head side to side (known as rooting) and moving their arms and legs.
When gravity pulls the mother or breastfeeding parent and baby apart, this movement of arms, legs, and head can be interpreted as the baby saying ‘no’ to breastfeeding, or ‘fighting’ the breast. Both the parent and baby can become distressed, and this can lead to a shorter breastfeeding relationship (Coulson, 2012).
With laid-back breastfeeding, the mother or breastfeeding parent reclines, and the baby is laid on their body. Gravity works with the breastfeeding parent and baby, holding them together. The baby is supported, but not held firmly, and is able to move towards the breast.
This position can be tried in bed, on a sofa or reclining gently in a chair supported with pillows or cushions. It is relaxed and comfortable for both, and reduces common breastfeeding problems (Coulson, 2012; Milinco et al, 2020).
A useful position for a fast milk flow and larger babies
A fast milk flow could be due to a large supply of breast milk. This can make the baby cough, splutter and come off the breast, which could look like symptoms of reflux.
Laid-back feeding, where the baby is more in control, helps with a fast milk flow, as gravity works against the flow of the milk. So it’s worth trying this before looking for other solutions.
It could also be useful with larger or older babies as it’s not necessary to hold the child’s weight with your arms.
Cradle
This is a position often seen when out and about, and as babies get bigger. It is referred to as ‘cradle’ hold if the supporting arm is on the same side as the breast being used. If the opposite arm is used, then it’s called ‘cross-cradle’.
- The baby lies across the parent’s lap
- The mother or breastfeeding parent’s arm supports the baby’s body, but the baby’s head is not held
- The baby’s body is tucked in close
- The baby’s ear, shoulder and hip are in a straight line (NHS Start for Life, no date b)
It may be more comfortable to have feet resting on a stool, to avoid leaning over the baby (NHS Start for Life, no date b).
Lying down
Breastfeeding lying down can be relaxing and help get more rest. It might also be useful after a caesarean birth or stitches (NHS Start for Life, no date b).
In this position, the mother or breastfeeding parent lies on their side with their bottom arm above the baby’s head. They may like a pillow behind their back for support. If using a pillow under the head, make sure it is clear of the baby (NHS Start for Life, no date b).
- Clear any duvets or pillows from around the baby. A rolled-up blanket behind them may help hold them in place, but remove it after feeding
- The baby lies on their side, facing the mother or breastfeeding parent and very close to their body
- The baby’s nose is in line with the nipple, and their ear, shoulder and hip are in a straight line
- The parent will need to guide the baby to the breast (NHS Start for Life, no date b)
Supported at the side
Holding the baby under the arm may be suggested after caesarean birth, to avoid pressure on the wound. This position can also be useful when feeding two babies at the same time (La Leche League GB, no date).
However, it can be difficult to maintain this position as the baby’s weight is being taken by the mother or breastfeeding parent’s hand. In this case, a pillow or pillows could be used to support the baby or babies' weight.
Make sure that the baby or babies' feet aren't touching anything, such as the back of the chair, as this will activate their stepping reflex and they will push away from the breast.
Babies soon outgrow this position, and it doesn’t allow them to use their instincts and reflexes to attach on to the breast.
What’s different for premature babies?
Neonatal staff will support parents with the feeding method that is most appropriate for their baby.
Babies need to co-ordinate sucking, swallowing and breathing to breastfeed. They may not learn this until after 34 weeks of pregnancy (NHS, 2022 b).
Babies who are born earlier than this may need to be fed through a tube with expressed milk to start with. The tube will be inserted through their mouth or nose and into their stomach (NHS, 2022 b).
These babies can later transition from tube feeding to breastfeeding.
Some very small or sick babies will be fed nutrients directly into a vein (NHS, 2022 b).
What is a lactation aid?
A lactation aid, sometimes called a supplemental nursing system, or SNS, can be used to help breastfeeding. A tiny tube is taped on next to the nipple, through which the baby can receive expressed breastmilk or formula as well as milk from the breast.
This gives them enough milk while they get used to breastfeeding (NHS, 2022 b). It is an alternative to giving a top up feed via a bottle.
Breastfeeding as the baby grows
As the baby grows, they become more active in getting themselves into position, and they're longer and heavier. So the breastfeeding positions may need to adjust to continue to feed comfortably and effectively.
Our NCT Breastfeeding Counsellors offer support with finding positions that suit you and your baby.
Breastfeeding Network (no date) How to breastfeed. https://www.breastfeedingnetwork.org.uk/breastfeeding-information/getti… [7 Jul 25]
Coulson S. (2012) Biological nurturing: the laid-back breastfeeding revolution Midwifery today. 101. https://midwiferytoday.com/mt-articles/biological-nurturing/ [1 Jul 25]
La Leche League GB. (no date) Positioning and attachment. https://laleche.org.uk/positioning-attachment/ [7 Jul 25]
Milinco M, et al. (2020) Effectiveness of biological nurturing on early breastfeeding problems: a randomized controlled trial. Int Breastfeed J. 15(1):21. https://doi.org/10.1186/s13006-020-00261-4
NHS (2022 a) Breastfeeding: positioning and attachment. https://www.nhs.uk/baby/breastfeeding-and-bottle-feeding/breastfeeding/… [27 Jun 25]
NHS (2022 b) Breastfeeding your premature baby. https://www.nhs.uk/baby/breastfeeding-and-bottle-feeding/breastfeeding/… [27 Jun 25]
NHS Start for Life (no date a) Latching on. https://www.nhs.uk/start-for-life/baby/feeding-your-baby/breastfeeding/… [1 Jul 25]
NHS Start for Life (no date b) Breastfeeding positions. https://www.nhs.uk/start-for-life/baby/feeding-your-baby/breastfeeding/how-to-breastfeed/breastfeeding-positions/ [1 Jul 25]
NICE (2021) Postnatal care. https://www.nice.org.uk/guidance/ng194/ [27 Jun 25]











