Some pregnancy discomforts are more of a concern than others. Here’s a rundown of what to expect, and when to get medical help. To make it easier to find what you’re looking for, we’re starting at the top of the body and working down.
Discomforts like carpal tunnel, cramp and restless legs are most common at night and more information can be found in our article on sleep in pregnancy. Those to do with bleeding and vaginal discharge are also in a separate article.
Head
Headaches
Headaches are common in early pregnancy, usually getting better as the pregnancy continues. They can be uncomfortable for the woman or pregnant person but don’t harm the baby (NHS, 2024a).
Some headache symptoms might be a sign of pre-eclampsia (NHS, 2024a).
What can relieve symptoms?
It might help to (NHS, 2024a):
- Drink plenty of water to stop dehydration
- Get enough sleep
- Find something that helps you relax, such as yoga or hypnobirthing (NCT Antenatal course bookers can access our exclusive videos and guides)
- It is safe to take paracetamol in pregnancy, though take it for the minimum time possible
Nosebleeds
Nosebleeds, also known the medical name epistaxis, are common in pregnancy. They aren’t usually a cause for concern (NHS, 2024b).
They are a result of hormonal changes and increased blood flow during pregnancy (NHS, 2024b).
Talk to your GP or midwife if you’re worried about nosebleeds. Frequent nosebleeds during pregnancy might sometimes mean a higher chance of bleeding after birth (Dugan-Kim et al, 2009). They might also suggest a rare clotting disorder (Andorfer et al, 2022).
Get in touch with the GP or midwife straight away if the bleeding won’t stop (NHS, 2024b).
Excessive saliva (ptyalism gravidarum)
Excessive saliva, also called ptyalism gravidarum (PG), is when the body makes too much saliva in pregnancy. The saliva produced is bitter and difficult to swallow, often triggering a retching reflex (Morton, 2024).
It’s most likely in the first trimester of pregnancy. It’s thought to be the body’s attempt to balance out acid caused by sickness and vomiting in the first trimester (Migliario et al, 2021).
PG is related to extreme sickness and vomiting.
Symptoms can be distressing and come on quickly. More than 9 out of 10 people who experience them feel them within eight weeks of pregnancy.
PG usually gets better on its own in the second trimester, although it can last until the baby is born. It doesn’t continue after the birth (Morton, 2024).
PG can cause (Morton, 2024):
- disrupted sleep and tiredness
- anxiety and depression
- loss of appetite and weight loss
What can relieve symptoms?
Although symptoms can’t be resolved, it might help to (Morton, 2024):
- spit out into a tissue or cup
- suck hard sweets
- chew gum
- use alkaline mouthwash
Some people with PG crave the sensation of eating earth.
Bleeding gums
Hormones during pregnancy can lead to inflamed and bleeding gums, as they’re more susceptible to plaque [plack]. It might also be called pregnancy gingivitis or gum disease (NHS, 2022a).
What can relieve symptoms?
It can help to practice good dental hygiene (NHS, 2022a):
- Keep teeth and gums healthy by brushing twice a day for two minutes each time
- Floss at least once a day
- Avoid sugary drinks and foods as much as possible, and keep them for mealtimes
- Snack on whole fruit or yoghurt rather than sugary foods
- Stop smoking
If suffering from pregnancy sickness, rinse the mouth with water after being sick. Don’t brush teeth for an hour or so as they will be softened by stomach acid (NHS, 2022a).
NHS dental healthcare is free during pregnancy and for the first year of the baby’s life. Apply for a maternity exemption certificate (MatEx) to get it. Ask a doctor, nurse or midwife for form F8. The pregnant woman or person completes the first two parts of the form. This then needs to be signed by the doctor, nurse or midwife (NHS, 2022a).
Always tell the dentist about the pregnancy during visits (NHS, 2022a).
Abdomen
Heartburn, indigestion and acid reflux
Heartburn and acid reflux are also called indigestion. Acid from the stomach can irritate the stomach lining up as far as the throat (NHS, 2023a).
Heartburn and acid reflux often start after the first trimester of pregnancy. It can be uncomfortable and distressing. However, it is unlikely to cause any harm (Phupong & Hanprasertpong, 2015).
They can be the result of (NHS, 2023a):
- the baby pressing against the stomach
- hormonal changes
- the muscles between the stomach and gullet relaxing, allowing acid to come back up
Heartburn and acid reflux might be felt as (NHS, 2023a):
- burning or pain in the chest
- feeling uncomfortably full or bloated
- being sick
- burping
Heartburn and acid reflux are more common if you had indigestion before pregnancy. They are also more likely if you have been pregnant before (NHS, 2023a).
What can relieve symptoms?
It can help to (NHS, 2023a):
- eat smaller meals more often, rather than three big meals a day
- avoid eating within three hours of going to bed
- cut down on rich, spicy or fatty foods
- cut down on drinks containing caffeine
- avoid alcohol
- stop smoking
Talk to your midwife or GP if making these changes doesn’t help the indigestion (NHS, 2023a).
Some prescription medications might make indigestion worse for some people, so talk to your GP about an alternative. Don’t stop taking prescribed medication without talking to a doctor (NHS, 2023a).
Medicine for indigestion
Medication with antacids helps reduce heartburn and acid reflux. They neutralise the stomach acids. However, always check with the pharmacist which ones are safe to use during pregnancy (NHS, 2023a).
Don’t take antacid within two hours of folic acid or iron supplements, as it can stop them being absorbed (NHS, 2023a).
Medicines called alginates can stop the acid coming back up your gullet (NHS, 2023a).
What about alternative remedies?
Some people find acupuncture helps them to eat and sleep better. It has no side effects (Phupong & Hanprasertpong, 2015).
‘Morning’ sickness and nausea
Nausea and vomiting in pregnancy is very common. Despite often being called ‘morning’ sickness, it can happen at any time of the day (NHS, 2024c).
Although unpleasant, it usually goes away by week 16 to 20 of pregnancy. It does not affect the baby or babies (NHS, 2024c).
Severe sickness is called hyperemesis gravidarum (HG) (NHS, 2024c). The charity Pregnancy Sickness Support provides support and information for those suffering from HG.
There's a higher chance of sickness when (NHS, 2024c):
- it's the first pregnancy
- it's a pregnancy with twins and multiples
- there's a history of migraine headaches
- sickness in pregnancy runs in the family
- there is a Body Mass Index (BMI) of 30 or more
What can relieve symptoms?
Even if the sickness reduces appetite, it can help to (NHS, 2024c):
- eat small, frequent meals of plain foods throughout the day
- avoid foods or smells that bring on feelings of sickness
- take small sips of drinks like water frequently
- eat foods containing ginger
Tiredness can make nausea worse, so getting rest could help. Some people find acupressure (wearing a bracelet or band on the pressure points on the wrist) also helps (NHS, 2024c).
Medicine for pregnancy sickness
If the above measures don’t help, a doctor may prescribe an antihistamine to reduce sickness (NHS, 2024c). These usually treat allergies but can also be used to stop sickness.
Abdominal pain
Stomach pains or cramps in pregnancy are common and usually not serious (NHS, 2024d).
They might be a sign of:
- the ligaments which attach the uterus to the pelvis stretching to support the growing bump
- constipation or trapped wind
In later pregnancy, they may be a sign of Braxton Hicks contractions.
If the cramps don’t go away after resting, going to the toilet or passing wind, call the GP or midwife. This might be a sign of something more serious (NHS, 2024).
Call the maternity unit urgently if there is stomach pain and (NHS, 2024):
- vaginal bleeding
- regular cramping
- fluid or discharge from the vagina
- lower back pain
- wee is red or brown, or cloudy
- the pain is intense and doesn’t go away after 30 minutes.
Sometimes, stomach pain can be caused by miscarriage, ectopic pregnancy or pre-eclampsia. It could be a urinary tract infection (UTI) or the placenta coming away from the womb (NHS, 2024d).
It can also be a sign of premature labour. So, it’s important to call the maternity unit straight away if there’s a feeling something isn’t right or you’re concerned (NHS, 2024d).
Breathlessness
Breathlessness is a common experience in pregnancy. It is usually noticed after 27 weeks. There is no risk for the baby (HSE, 2023).
Breathlessness may happen as the body adapts to the growing baby. This might be more noticeable if carrying twins or more. It can also be due to the extra weight being carried (HSE, 2023).
Practising using the lungs effectively through yoga or similar gentle exercise can help.
When might shortness of breath be a concern?
Talk to the midwife if (Healthier together, no date):
- there is tiredness and palpitations as well as breathlessness, as it could be a sign of low iron levels in the blood
- breathlessness happens when sitting or standing still
Occasionally, breathlessness during pregnancy can be a sign of something serious. Call 999 or go to the Emergency department if (Healthier together, no date; NHS, 2024e):
- the breathlessness is severe, with gasping or choking
- the chest feels tight or heavy
- there is pain when breathing in deeply or coughing
- the pain spreads to the arms, back, neck or jaw
- the lips or skin turns very pale, blue or grey (on Black or Brown skin this can be easier to see on the palms of the hands)
- breathlessness happens when lying down, sitting or standing still
- you feel suddenly confused
Asthma and pregnancy
Pregnancy can make asthma symptoms worse, so talk to the GP if this happens (Healthier together, no date).
Blood clots and pregnancy
Pulmonary embolism is when there is a blood clot on the lung. It can happen in 1 in 1000 pregnancies (Healthier together, no date).
Reduce the risk by (Healthier together, no date):
- drinking enough fluids
- moving around often
- stopping smoking
- keeping a healthy weight
Faintness and pregnancy
Feeling faint is normal in pregnancy due to hormonal changes (NHS, 2024f).
- If you’re standing up, find somewhere to sit or lie on your side until you feel better
- If you feel faint after standing up quickly, remember to get up more slowly next time
- Feeling faint while lying on your back is a sign to turn onto your side.
Stretch marks

Stretch marks happen in most pregnancies. These are lines that appear on the skin of the stomach, the upper thighs and breasts. They vary according to skin colour, from silvery-white or pink to red to purple and brown (NHS, 2022b).
They might be itchy, but they aren’t harmful (NHS, 2022b).
There’s no strong evidence that using creams or oils can prevent stretch marks or reduce them after birth (NHS, 2022b).
Leaking nipples
It’s normal for nipples to leak milk during pregnancy. The breasts start producing milk months before the baby is born (NHS, 2024g).
Some women and pregnant people find they need to start using breast pads earlier than expected.
Call the GP or midwife if the milk has blood in it (NHS, 2024g).
Below the waist
Back and pelvic pain
During pregnancy the ligaments in the body get softer and stretch to prepare for labour. This is a common cause of back pain (NHS, 2024h).
Paracetemol can be taken during pregnancy for mild back pain. For back or pelvic pain that won’t go away, an obstetric physiotherapist may be able to help (NHS, 2024). Ask your midwife to refer you, or in some areas you can self-refer by contacting the hospital.
Call the GP or midwife urgently if (NHS, 2024h):
- back pain happens during the second or third trimester as this might be early labour
- there is also a fever as well as back pain
- it hurts when having a wee, or there is blood coming from the vagina
- there is pain under the ribs on one or both sides
If there is back pain and feeling is lost in one or both legs, or bottom or genitals, call 999 or go to the Emergency department.
Doing yoga or other exercise during pregnancy can be helpful to each aches and pains.
For some women and pregnant people, the pain includes the whole pelvis. For others, it could be to do with the position of the baby.
Swollen ankles, feet and fingers
Pregnant women and people often experience swelling in their ankles, feet and fingers (NHS, 2024i).
This happens because the pregnant body needs to hold more water than normal. This extra water can settle in the lowest parts of the body during the day (NHS, 2024i).
Because of this, it might get worse as the day goes on, particularly if it’s a hot day or after long periods of standing. It might increase towards the end of pregnancy (NHS, 2024i).
The growing pressure of the womb can also affect blood flow, leading to swelling in the legs, ankles and feet (NHS, 2024i).
Gradual swelling is normal, but if the swelling happens suddenly, it might be a sign of preeclampsia. Contact the midwife or maternity unit immediately if this happens (NHS, 2024i).
Things that might help (NHS, 2024i):
- Avoid standing or being static for long periods
- Regularly rest with feet raised up
- Wear comfortable clothes and footwear
- Foot exercises can improve circulation
- Drinking less will not reduce the fluid and could lead to dehydration.
Peeing all the time
During pregnancy, it’s common to need to pee often. And in late pregnancy the baby’s head might be pressing down on the bladder. When you go to the toilet, leaning forwards can help empty the bladder (NHS, 2024f).
It’s important to stay hydrated with caffeine-free and non-alcoholic drinks during the day. Nearer to bedtime you could reduce liquids. However, bear in mind that dehydration can cause leg cramps (NHS, 2024f; NHS, 2023).
If there is blood or pain when peeing, then contact the GP as it might be a sign of a urine infection (NHS, 2024f).
Incontinence
When sneezing, coughing, jumping or getting up from sitting, it’s common in pregnancy and after birth to wee slightly. This is most likely temporary, because the pelvic floor muscles relax to prepare for the birth of the baby (NHS, 2024f).
You can do exercises to protect against this being a long-lasting problem. Read about leaking urine in pregnancy in our article.
Constipation, haemorrhoids, and anal fissures
Constipation (when it is hard to have a poo) frequently happens in pregnancy. It can be helped by (NHS, 2024f):
- Eating foods high in fibre, like wholemeal bread, whole fruit (not smoothies), vegetables and pulses
- A healthy diet will also mean you can avoid iron supplements, which can make you constipated
- Drinking plenty of water
- Doing exercise
Piles (Haemorrhoids)
Constipation can cause haemorrhoids, commonly known as piles. These are swollen blood vessels inside the anus (bottom). Sometimes they are large enough to push through the anus so they can be seen from outside. Although anyone can get piles, pregnancy might be the first time they are experienced (NHS, 2024j).
Piles can be uncomfortable, itchy and sore, and can be painful when doing a poo. There might be mucus discharge, and bright red blood (NHS, 2024j).
Straining on the toilet can make piles worse. So, the best tip is to reduce the chance of constipation (NHS, 2024).
Clean the area by patting with moist tissue after having a poo. A cold cloth held against the piles can ease the pain. Ask the midwife, doctor or pharmacist for a pregnancy-suitable treatment to help soothe the area (NHS, 2024).
Anal fissure
Anal fissures are tears or sores that develop near the anus (bottom) (NHS, 2021).
Constipation usually causes these issues when a large or hard poo tears the lining of the anal canal (NHS, 2021).
An anal fissure might cause:
- a sharp pain when having a poo, then a burning pain afterwards
- a small amount of bright red blood when having a poo
See a GP if you notice these symptoms, so they can rule out other problems and provide soothing ointment. Anal fissures usually get better within a few weeks (NHS, 2021).
Varicose veins
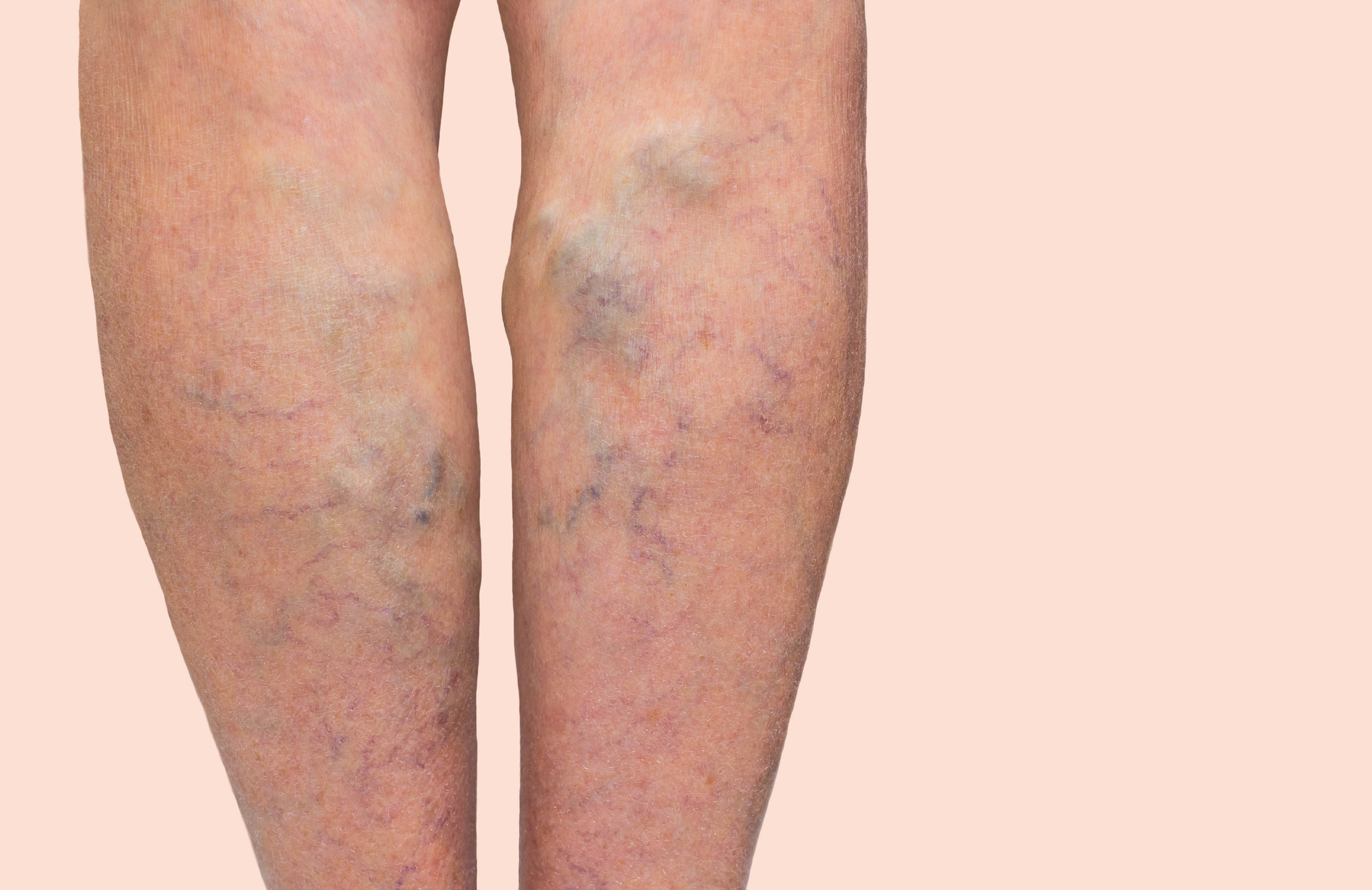 Varicose veins are swollen, twisted veins which bulge out from under the skin (NHS, 2024k). Lots of pregnant women and people get varicose veins in the first trimester of pregnancy (Circulation Foundation, no date). These are usually on the legs but can be in the vulva (around the vaginal opening) (NHS, 2024f).
Varicose veins are swollen, twisted veins which bulge out from under the skin (NHS, 2024k). Lots of pregnant women and people get varicose veins in the first trimester of pregnancy (Circulation Foundation, no date). These are usually on the legs but can be in the vulva (around the vaginal opening) (NHS, 2024f).
Pregnancy hormones and more blood make the veins bigger. As the womb grows there is also more pressure on veins (Circulation Foundation, no date).
Varicose veins usually get better within a few months after the baby is born. However, after each pregnancy they may be less likely to go away (Circulation Foundation, no date).
It can help to (NHS, 2024f):
- not stand for a long time
- keep legs uncrossed
- sit or lie down with the legs raised up
- do gentle exercise to improve blood circulation
- talk to a pharmacist or GP about compression stockings to improve blood flow
- try to keep a healthy weight
- not smoke
Varicose veins often run in families and aren’t usually serious (Circulation Foundation, no date; NHS, 2024k).
It is rare for varicose veins to bleed after being knocked. Firm pressure will help it stop bleeding. Then see a doctor for treatment (Circulation Foundation, no date).
Varicose veins might be associated with deep vein thrombosis (DVT). So, if there is pain in the leg or skin damage around the ankle, see a GP and mention DVT (Circulation Foundation, no date).
Andorfer, K. E. C., Seebauer, C. T., Dienemann, C., Marcrum, S. C., Fischer, R., Bohr, C., & Kühnel, T. S. (2022). HHT-Related Epistaxis and Pregnancy—A Retrospective Survey and Recommendations for Management from an Otorhinolaryngology Perspective. Journal of Clinical Medicine, 11(8), 2178. https://doi.org/10.3390/jcm11082178
Circulation Foundation (no date) Varicose veins. https://www.circulationfoundation.org.uk/patient_info/veins/varicose-ve… [19 Mar 25]
Dugan-Kim M, Connell S, Stika C, Wong CA, Gossett DR (2009) Epistaxis of Pregnancy and Association With Postpartum Hemorrhage. Obstetrics & Gynecology 114(6):p 1322-1325, https://doi.org/10.1097/AOG.0b013e3181bea830
Healthier Together (no date) Breathlessness. https://www.what0-18.nhs.uk/pregnant-women/concerns-during-pregnancy/ov… [18 Mar 25]
Migliario M, Bindi M, Surico D, De Petrini A, Minsenti S, Pazzotti F, Mele B, Foglio Bonda PL (2021) Changes in salivary flow rate and pH in pregnancy. European Review for Medical and Pharmacological Sciences. 25: 1804-1810. https://doi.org/10.26355/eurrev_202102_25074
Morton A, He JW. (2024) Ptyalism gravidarum. Obstet Med. 21:1753495X241290668. https://doi.org/10.1177/1753495X241290668
NHS (2021) Anal fissure. https://www.nhs.uk/conditions/anal-fissure/ [19 Mar 25]
NHS (2022a) Bleeding gums in pregnancy. https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/bleedin… [14 Mar 25]
NHS (2022b) Stretch marks. https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/stretch… [19 Mar 25]
NHS (2023a) Indigestion and Heartburn in pregnancy. https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/indiges… [14 Mar 25]
NHS (2023b) Leg cramps. https://www.nhs.uk/conditions/leg-cramps/ [14 Apr 25]
NHS (2024a) Headaches in pregnancy. https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/headach… [14 Mar 25]
NHS (2024b) Nosebleeds in pregnancy. https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/noseble… [14 Mar 25]
NHS (2024c) Vomiting and morning sickness. https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/vomitin… [14 Mar 25]
NHS (2024d) Stomach pain in pregnancy. https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/stomach… [18 Mar 25]
NHS (2024e) Shortness of breath. https://www.nhs.uk/conditions/shortness-of-breath/ [18 Mar 25]
NHS (2024f) Common health problems in pregnancy. https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/common-… [18 Mar 25]
NHS (2024g) Leaking from your nipples. https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/leaking… [19 Mar 25]
NHS (2024h) Back pain in pregnancy. https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/back-pa… [17 Mar 25]
NHS (2024i) Swollen ankles, feet and fingers in pregnancy. https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/swollen… [18 Mar 25]
NHS (2024j) Piles in pregnancy. https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/piles/ [19 Mar 25]
NHS (2024k) Varicose veins. https://www.nhs.uk/conditions/varicose-veins/ [19 Mar 25]
Phupong V, Hanprasertpong T. (2015) Interventions for heartburn in pregnancy. Cochrane Database of Systematic Reviews, Issue 9. Art. No.: CD011379. https://doi.org/10.1002/14651858.CD011379.pub2







